E-LOG MEDICINE
49/M WITH DIABETIC KETOSIS SECONDARY TO ?ACUTE GASTROENTERITIS
This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent.
Name : R.KOUSHIK CHANDRA
Roll no:108
A 49 Year old male, autodriver by occupation , came to casualty on 24th June 2023 with chief complaints of
CHIEF COMPLAINTS:
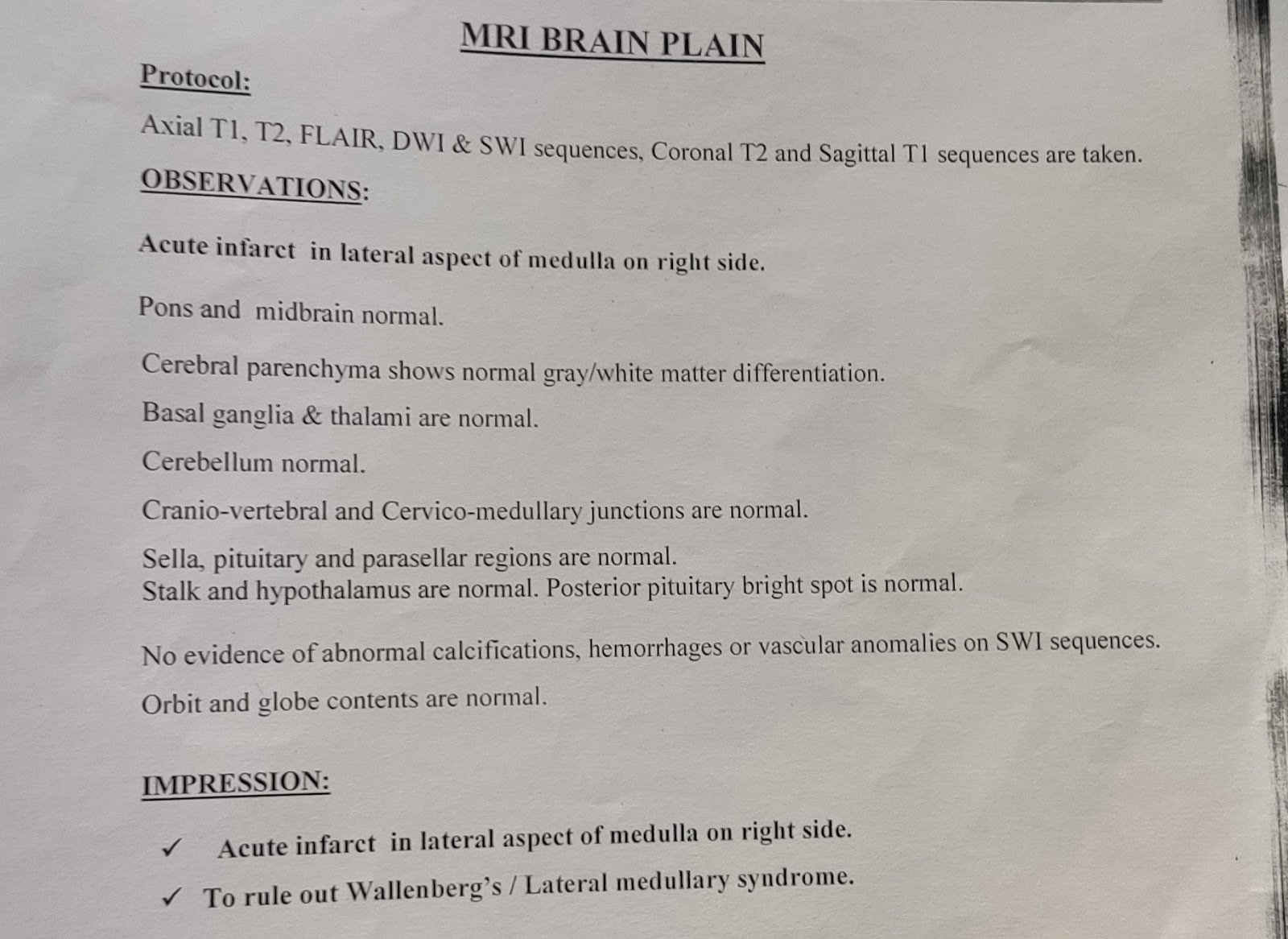
Giddiness since one week and pain and weakness in the right lower limb since one week.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 5 days ago then he developed Giddiness which is sudden in onset, gradually progressive.
C/o Vomitings 4-5 episodes, watery, non-projectile, bilious with food particles on the same day of giddiness. Not Blood tinged. Relieved with medications.
C/o Loose stools: 4-5 episodes, watery, non blood stained, non-mucoid, non- foul smelling since the day of joining.
C/o Pain in Right side of body along with weakness of Right lower limb, one week back,
C/o Facial puffiness since one week.
C/o pain on the forehead radiating to right side of the face.
No C/o Fever, pain abdomen, decreased urinary output, pedal edema.
DAILY ROUTINE
The patient is a Farmer and Autodriver
- 4AM: Wakes up and goes to farm(occasionally)
- 8AM: Drinks Tea
- 9AM: He eats Rice
- 10AM- 1PM: Goes for driving Auto
- 1PM: Eats Lunch- Rice with dal
- 2PM: Takes a nap and wakes up at 4PM
- 4PM: Goes for driving Auto
- 6:00: Tea and soft drink
- 8PM: Dinner
- 9PM: The patient goes to bed by 9PM
PAST HISTORY :
Patient went to a hospital 1 month back with C/o headache, giddiness and was diagnosed as hypertension and put on medications.
Patient is a known case of DM II since 13 years and is on medication.(GLIMI-M4 Forte PO/OD)
The patient was operated for haemorrhoids 20 years back
Not a known case of CAD, Bronchial asthma, Epilepsy, TB.
PERSONAL HISTORY
DIET - Mixed
APPETITE- Decreased since one week
SLEEP - Adequate
BOWEL AND BLADDER- Regular
ADDICTIONS - alcoholic since 10 years.Stopped consumption 6 years back.
Chewing tobacco since 20 years.
FAMILY HISTORY
No relevant family history
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative; well oriented to time,place and person moderately built and well nourished.
No icterus, clubbing, cyanosis, lymphadenopathy, edema.
VITALS:
- BP: 120/80 mmHg
- PULSE : 82 Bpm
- RESPIRATORY RATE: 14cpm
- TEMPERATURE: Afebrile



Comments
Post a Comment