E-LOG MEDICINE
R.KOUSHIK CHANDRA
108
This is an online e-log platform to discuss case scenario of a patient with their guardians permission.
I have been given this case to solve in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including, history, clinical findings ,investigations, come up with a diagnosis and treatment plan.
Chief complaints:
A 65 yr old male came with chief complaints of:
Swelling of both legs upto ankle since 10 days
Facial puffiness since 10 days
Slurred speech,dryness of mouth and shortness of breath since 10 days.
History of presenting illness:
Patient was apparently asymptomatic 5 years back (2018) then he developed swelling in both legs upto ankle and shortness of breath for which he went to hospital there he was diagnosed with hypertension and was given medication.
Later he consulted another doctor he told them to stop the medication and he told that the hypertension was due to a problem in the kidney and was medication which the patient used for one month.
3 yrs back (2020) patient again had similar complaints along with slurring of speech and dryness of mouth after talking for 4-5 min for which he consulted a doctor and he told that there was reduction in size of the right kidney and creatinine was raised (2.3).
Medication was given and symptoms subsided.
10 days back before joining here patient had swelling of legs upto ankle and shortness of breath on exertion(MMRC) and went to hyd in the morning and he was advised to undergo dialysis.
On the way to our hospital he had 4 episodes of vomiting which is watery,non projectile,non bilious,no food particles.
No history of headache,fever,stools,pain in the abdomen,burning micturiton ,decreased urine output .
Past history :
Known case of hypertension since 5 yrs
Patient undergone hydrocoele operation 10 yrs back.
No history of diabetes,asthma,epilepsy,cad,cva,tb
Personal history :
Sleep: adequate
Appetite:decreased since 10 days
Diet:mixed
Addictions:no addictions
Bowel and bladder:regular
Family history:
No significant family history
General examination:
Patient was conscious,coherent,cooperative well oriented to time,place and person
Moderately built ,moderately nourished
Vitals:
Pulse:92 beats/ min
Afebrile
RR: 14 times/ min
BP:
Mild pallor
No icterus,cyanosis,clubbing,lymphadenopathy,pedal edema
Systemic examination :
CVS:
S1 S2 heard ,no murmurs
CNS:
No focal neurological deficit found
RR:
Normal vesicular breath sounds heard
Trachea Central
B/l air entry +
Per abdomen:
No palpable mass detected
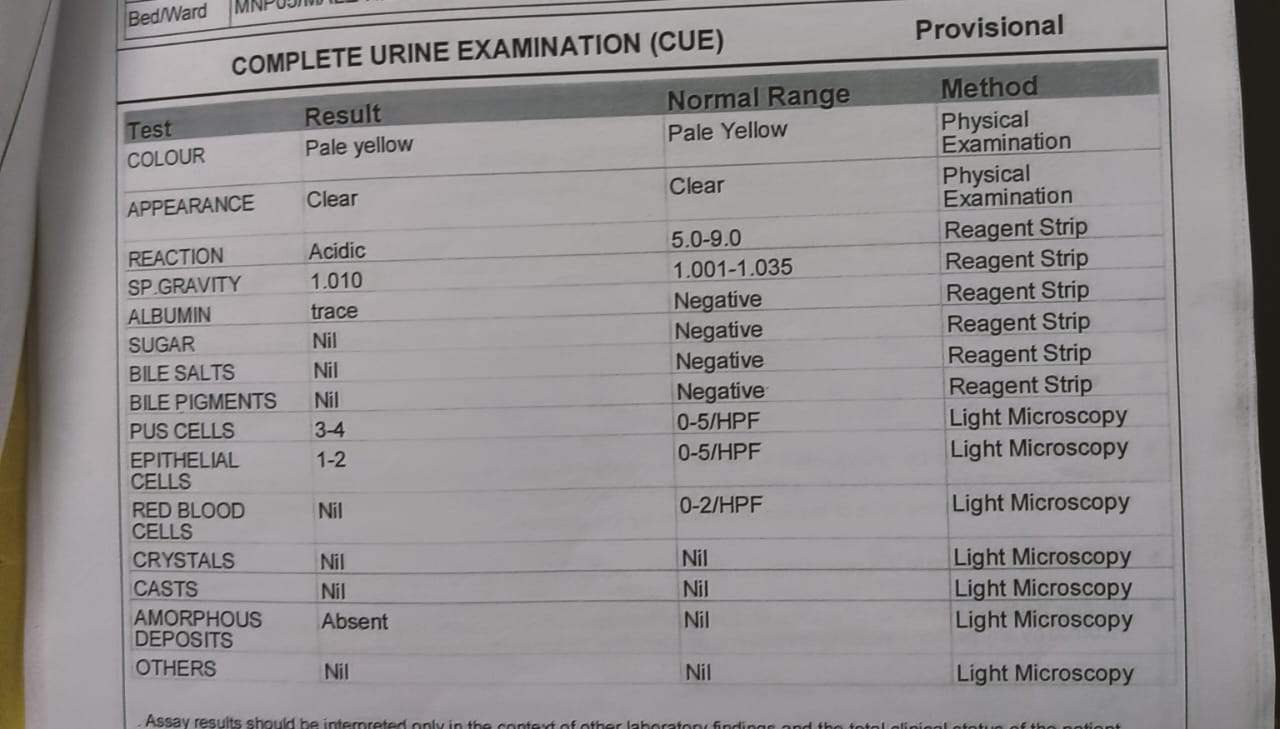
Investigations:
Provisional diagnosis:
CKD
TREATMENT:
Fluid restriction less than 2 litres/day
Salt restriction less than 2 GM's/day
Tab.Nodosis 500 mg po/bd
Tab.lasix 40 mg po/bd
Tab.orofer po/od
Tab.shelcal po/od
Cap.bio-d3 po/once a week
Hemodialysis





















Comments
Post a Comment